Definition
Late-stage diabetic foot is a severe complication associated with chronic diabetes. This condition encompasses a spectrum of issues, from ulcers and infections to the more severe gangrene.
Causes
consequence of prolonged high blood sugar levels, which inflict damage on blood vessels and nerves, especially in the extremities.
The damage to nerves, known as peripheral neuropathy, results in patients losing sensation in their feet. This numbness, combined with reduced blood flow due to damaged blood vessels, can lead to non-healing ulcers.
PATHOPHYSIOLOGY OF LATE-STAGE DIABETIC FOOT
1- Neuropathy
2- Ischemia
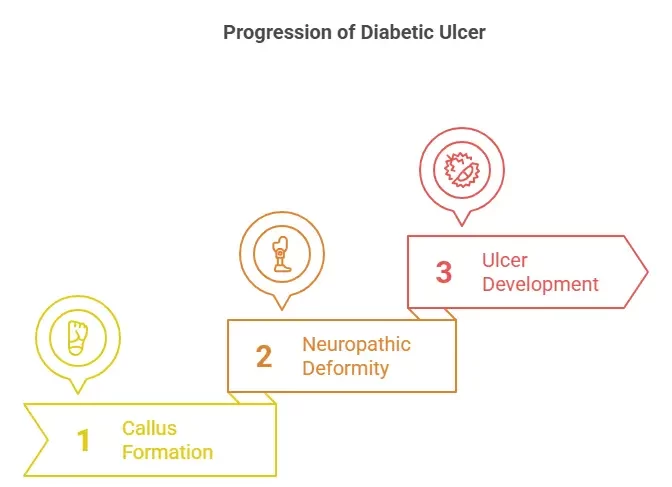
THE DEVELOPMENT OF A DIABETIC ULCER USUALLY PROGRESSES IN THREE STAGES
stage one: the formation of a callus, resulting from
neuropathy.
stage two: Motor neuropathy causes physical deformity of the foot, and sensory
neuropathy leads to ongoing trauma.
stage three: Frequent trauma to the callus results in subcutaneous hemorrhage,
which eventually erodes and becomes an ulcer.
EPIDEMIOLOGY
Global Prevalence:
1- Estimated at 6.3% of people with diabetes.
2- More common in older adults and those with longer diabetes duration.
3- Risk Factors include neuropathy, vascular disease, foot deformities, poor glycemic control, smoking, and obesity.
4- Complications: Ulceration, infection, gangrene, and amputation.
Causes of Diabetic Foot:
1- Neuropathy: Nerve damage reduces sensation, increasing injury risk.
2- Vascular Disease: Impairs wound healing and raises infection risk.
3- Foot Deformities: Increase pressure on areas, leading to ulceration.
4- Poor Glycemic Control: Damages nerves and blood vessels.
5- Smoking and obesity also contribute to foot problems.
Prevalence in GCC and Middle East:
1- Estimated prevalence: Around 10% of people with diabetes in the GCC region.
2- Risk factors include lifestyle factors like physical inactivity, unhealthy diet, and footwear choices.
Significance:
1- Major public health problem: Leading cause of hospitalization and amputation in people with diabetes.
2- Significant cost burden: Costs billions of dollars in healthcare expenditures annually.
3- Impact on quality of life: Leads to pain, mobility limitations, social isolation, and psychological distress.
INNOVATION
CUSTOM BIOENGINEERED GRAFTS: One of our groundbreaking innovations is the
development of custom bioengineered grafts.
1- Deliver Essential Growth Factors: Our grafts are infused with vital
growth factors that promote wound healing. These growth factors
stimulate cell proliferation and differentiation, essential processes in
wound repair
2- Seamless Integration: Unlike traditional grafts, our bioengineered
grafts are designed to integrate seamlessly with the patient’s existing
tissue. This ensures that there’s no rejection and that the graft works in
harmony with the body
3- Accelerated Healing: By delivering growth factors directly to the affected
area and ensuring seamless integration, our grafts accelerate the healing
process. This is crucial for late-stage diabetic foot patients, where timely
wound healing can prevent complications and improve outcomes.
the effects of bio engineering on diabetic foot
1- decrease amputation rates
2- improve quality of life
3- REDUCTION IN LONG-TERM HEALTHCARE COSTS
Case Studies (Before&After)