Definition
the array of techniques and practices employed to improve the appearance and condition of scars following injury, surgery, or other causes of skin trauma
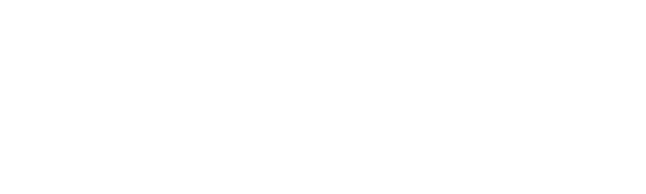
TYPES OF SCARS
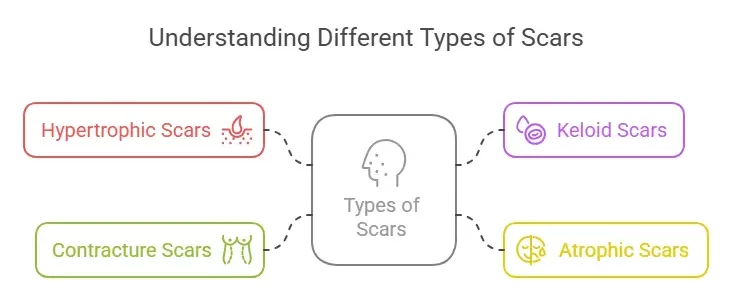
PATHOPHYSIOLOGY OF SCAR FORMATION
EPIDEMIOLOGY
• Saudi Arabia: %72 prevalence of scars; burns
(%42), surgery (%38), trauma (%82 .)%20
dissatisfaction with appearance.
• Qatar: %2.6 prevalence of keloid scars,
characterized by raised, thickened areas.
• Global Prevalence: Estimated at %60-50.
• GCC and Middle East: Similar prevalence,
with burns and trauma as common causes.
• Psychological Impact:
Significant, including self-consciousness, social avoidance, depression, and anxiety.
• Common Causes:
Burns, surgery, trauma, acne, chickenpox.
• Physical Health:
Aids in healing, reduces discomfort, and prevents mobility issues.
• Appearance Enhancement:
Improves aesthetic look, making scars less noticeable.
• Psychological Well-being:
Boosts self-esteem and reduces social anxiety.
• Social and Professional Impact:
Enhances confidence in social and work environments.
• Prevention of Complications:
Minimizes long-term issues like hypertrophic scars or keloids.
• Personalized Treatment:
Offers tailored approaches based on individual scar characteristics.
• Advancements in Care:
Incorporates innovative, effective, and less invasive treatments.
• Economic Benefits:
Reduces long-term treatment costs for individuals and healthcare systems.
PROGRESSION STAGES OF SCAR MANAGEMENT
1- Initial SCAR MANAGEMENT:
• Timeframe: Immediately after injury until a few days later.
• Characteristics: The wound begins to heal through the body’s natural processes, involving hemostasis, inflammation, and the beginning of tissue proliferation.
• Management: Proper wound care is crucial at this stage to prevent infection and minimize future scarring. This includes cleaning, possibly suturing if necessary,
and protecting the wound.
2. Early Scar Formation:
• Timeframe: From a few days to a few weeks post-injury.
• Characteristics: The scar starts to form as the body produces new collagen fibers.
The scar may appear red, raised, and firm.
• Management: Continued wound care is important. Silicone gel sheets or ointments
may be introduced to keep the area hydrated and minimize excessive collagen buildup.
3. Scar Maturation:
• Timeframe: Several weeks to months after the injury.
• Characteristics: The scar begins to mature; collagen is remodeled, and the scar becomes flatter, softer, and paler.
• Management: This stage may involve interventions like pressure therapy, especially for burn scars, to help flatten and soften the scar. Massage and
moisturization can also be beneficial.
4. Established Scar:
• Timeframe: 6 months to 2 years post-injury.
• Characteristics: The scar is fully formed and has completed most of its healing and remodeling. However, scars can continue to change subtly for years.
• Management: Treatment at this stage may include more invasive procedures if the scar is problematic. These can include laser therapy,
steroid injections, or surgical revision for aesthetic or functional improvement.
INTEGRATION OF TISSUE ENGINEERING FOR SCAR MANAGEMENT
1. Immediate Post-Injury (72-0 hours)
Tissue Engineering Interventions:
• Application of bioactive scaffolds that release growth factors and cytokines to promote healthy tissue regeneration and minimize inflammatory responses.
• Use of hydrogels or other biomaterials to protect the wound and maintain a moist environment, which is crucial for optimal healing.
2. Early Post-Injury (72 hours to 3 weeks)
Tissue Engineering Interventions:
• Implementation of advanced cell therapies, such as the application of fibroblasts or keratinocytes, to promote proper skin formation.
• Continued application of bioactive scaffolds, possibly integrated with additional growth factors to support
3. Intermediate Stage (3 weeks to 3 months)
Tissue Engineering Interventions:
• Application of 3D bioprinted skin grafts or tissue-engineered constructs for larger or more complex wounds.
• Use of scaffolds that gradually degrade while continuing to release
Case Studies (Before&After)